Verruca Plana Pathology
Comprehensive histopathology of flat warts (verruca plana): Key features, diagnosis, and differentials for dermatologists.
Verruca plana, commonly known as flat warts, are benign cutaneous lesions caused by specific human papillomavirus (HPV) types, primarily HPV-3, HPV-10, HPV-28, and HPV-41. These warts are characterized by their flat-topped, slightly elevated appearance and lack the hyperkeratotic, exophytic features of other viral warts like verruca vulgaris. Histopathologically, they exhibit subtle epidermal changes with diagnostic viral cytopathic effects.
Introduction
Verruca plana represents a distinct subtype of cutaneous viral warts, distinguished by minimal hypertrophic changes and a predominance of superficial epidermal involvement. Unlike the papillomatous architecture of common warts, flat warts show gentle undulations of the epidermis with prominent koilocytosis in the upper layers. This pathology page details the microscopic features, clinical correlations, differential diagnoses, and diagnostic considerations for verruca plana.
Clinically, verruca plana present as multiple small (1-5 mm), flat-topped, skin-colored to brownish papules, often on the face, dorsal hands, forearms, or shins. They are autoinoculable, spreading linearly via scratching or shaving (pseudo-Koebner phenomenon). While usually benign, they can persist and occasionally mimic dysplastic lesions, particularly in epidermodysplasia verruciformis (EV).
Histopathology
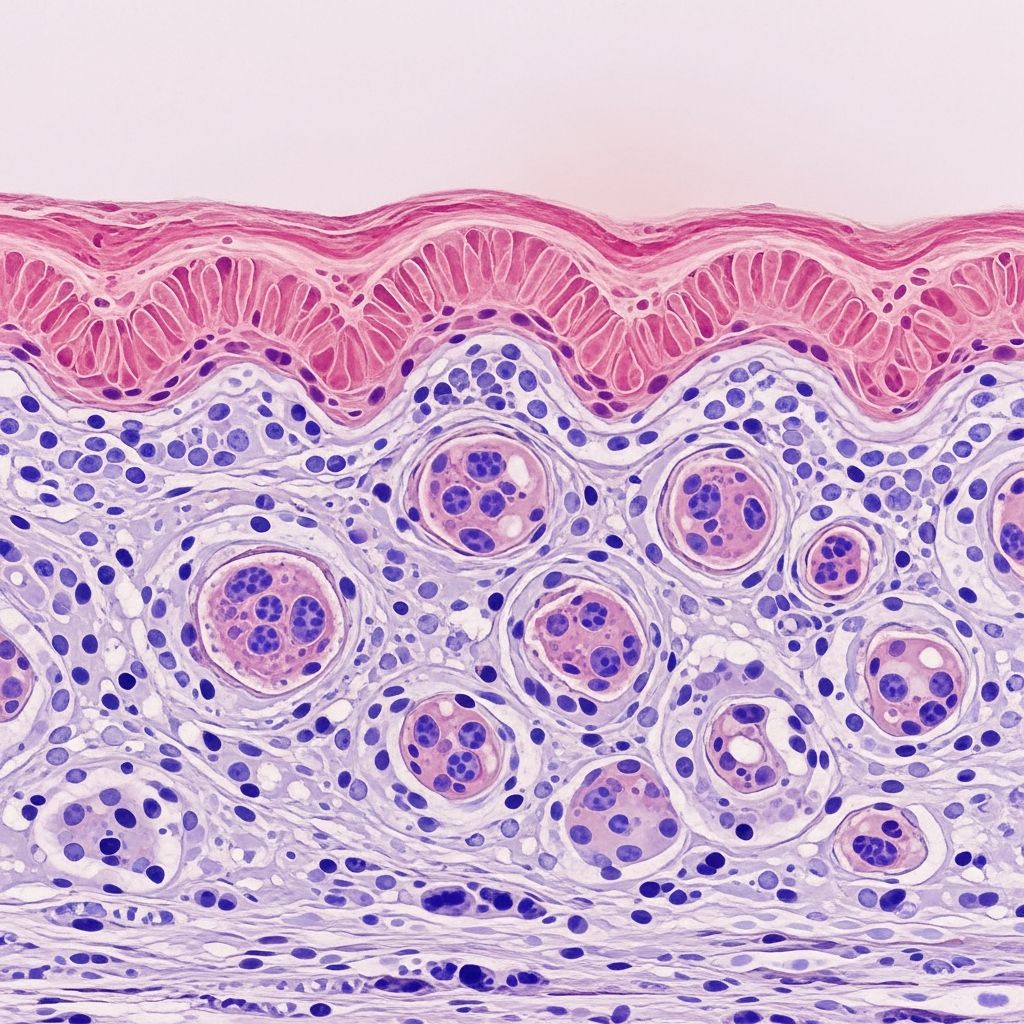
The hallmark of verruca plana is subtle epidermal hyperplasia with a flat or slightly undulating surface, lacking the marked papillomatosis and hyperkeratosis seen in verruca vulgaris. Key features include:
- Hypergranulosis: Thickened granular layer with coarse keratohyalin granules.
- Koilocytes: Vacuolated keratinocytes in the upper spinous and granular layers, featuring perinuclear halos, shrunken hyperchromatic nuclei, and amphophilic cytoplasm—often termed “bird’s-eye cells”.
- Mild acanthosis: Slight thickening of the spinous layer without elongated rete ridges.
- Parakeratosis: Focal retention of nuclei in the stratum corneum, less pronounced than in other warts.
- Blunted papillomatosis: Gentle surface undulations without finger-like projections.
In the granular layer, HPV-infected cells display coarse keratohyalin granules and perinuclear vacuoles surrounding wrinkled nuclei. These changes are most evident in the upper epidermis. Dilated capillaries may be present in dermal papillae, but vascular ectasia is minimal compared to plantar warts.
Microscopic Images Description
Low-power view reveals a flat epidermis with vague papillomatosis and hypergranulosis (Figure 1). Higher magnification highlights koilocytes with clear perinuclear halos and slightly enlarged, uniform nuclei (Figure 2). In some cases, focal epidermodysplasia verruciformis (EDV)-like changes coexist, showing blue-gray cytoplasm and nuclear atypia.
Cytopathic Effects
The HPV cytopathic effect is pathognomonic for verruca plana. Infected keratinocytes exhibit:
| Feature | Description | Layer Affected |
|---|---|---|
| Koilocytosis | Perinuclear clearing (halo) with pyknotic nucleus | Upper spinous/granular |
| Hypergranulosis | Thickened stratum granulosum | Granular |
| Basophilic inclusions | Small intranuclear inclusions (rare) | Granular |
| Amphophilic cytoplasm | Bird’s-eye appearance | Spinous |
These effects result from HPV replication in differentiating keratinocytes, disrupting normal maturation. PCR can confirm HPV subtypes, though not routinely needed for diagnosis.
Clinical Features
Flat warts are most common in children and young adults, with a female predominance due to shaving practices. Sites include:
- Face (especially beard area in males).
- Dorsal hands and forearms.
- Anterior shins (common in females).
- Linear arrangements from koebnerization.
Lesions are asymptomatic but cosmetically bothersome. Resolution often occurs spontaneously within 1-2 years via cell-mediated immunity.
Diagnosis
Diagnosis is primarily clinical, supported by dermoscopy showing pinpoint vessels without thrombi (unlike seborrheic keratosis). Biopsy is reserved for atypical or persistent cases. Routine H&E stain suffices; special stains or IHC are unnecessary.
Differential Diagnoses
Verruca plana must be distinguished from several mimics:
| Differential | Key Distinguishing Features |
|---|---|
| Verruca vulgaris | Marked papillomatosis, tiers of parakeratosis, thrombi in capillaries |
| Seborrheic keratosis | Horn cysts, pseudohorn cysts, no koilocytes; stuck-on appearance clinically |
| Lichen simplex chronicus | Hyperkeratosis, acanthosis, vertical collagen streaks; history of rubbing |
| Epidermodysplasia verruciformis (EDV) | Blue-gray cytoplasm, nuclear atypia; genetic predisposition |
| Actinic keratosis | Atypical keratinocytes throughout epidermis, solar elastosis |
| Molluscum contagiosum | Large eosinophilic inclusions (Henderson-Patterson bodies), not koilocytes |
Older verruca plana may lose viropathic effects, leading to overlap with verrucal keratosis.
Complications and Associations
- Autoinoculation via trauma.
- Rare malignant transformation in EV (HPV-5,8).
- Coexistence with lichen simplex chronicus from picking.
Treatment Considerations
Though not primarily a treatment page, pathology informs management. Refractory cases may require biopsy to exclude dysplasia. Options include cryotherapy, salicylic acid, or imiquimod, targeting HPV.
Frequently Asked Questions (FAQs)
Q: What causes verruca plana?
A: Infection with HPV types 3, 10, 28, or 41, entering via minor skin trauma.
Q: How do koilocytes appear under the microscope?
A: As keratinocytes with perinuclear halos, shrunken nuclei, and clear cytoplasm in the upper epidermis—diagnostic of HPV.
Q: Can verruca plana become cancerous?
A: Rarely; in epidermodysplasia verruciformis, specific HPV types increase squamous cell carcinoma risk.
Q: What’s the difference from common warts pathologically?
A: Flat warts lack papillomatosis and hyperkeratosis; show subtler changes with prominent koilocytes.
Q: Is biopsy always needed?
A: No, clinical diagnosis suffices; biopsy for atypical or non-resolving lesions.
References
- Verruca vulgaris (common wart) pathology — DermNet NZ. 2023. https://dermnetnz.org/topics/verruca-vulgaris-pathology
- Introduction to dermatopathology — DermNet NZ. 2023. https://dermnetnz.org/topics/introduction-to-dermatopathology
- Wart – StatPearls — NCBI Bookshelf, NIH. 2023-10-01. https://www.ncbi.nlm.nih.gov/books/NBK431047/
- Verruca plana (flat wart) under microscope histology pathology — YouTube (Pathology Review). 2023. https://www.youtube.com/watch?v=d_DjqM5osSc
- Viral wart — DermNet NZ. 2023. https://dermnetnz.org/topics/viral-wart
Read full bio of Sneha Tete