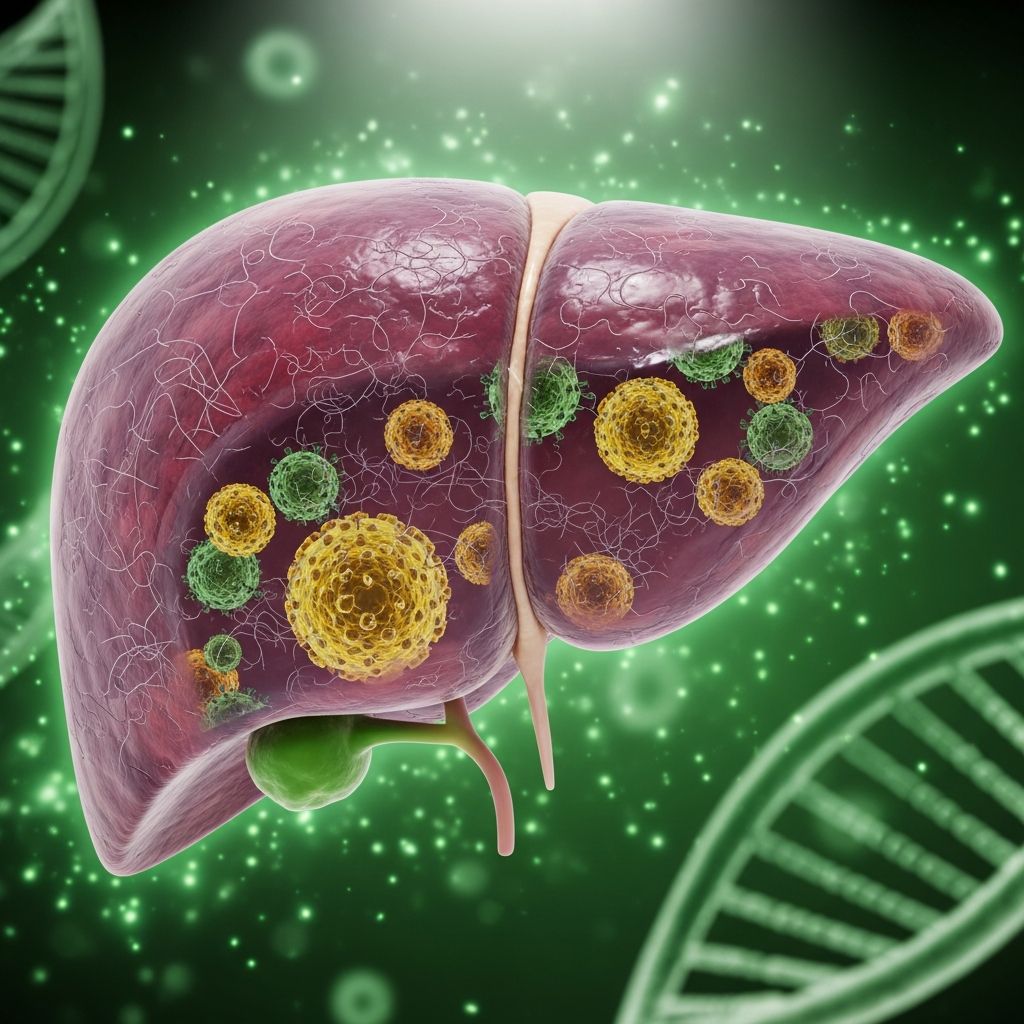
Viral Hepatitis
Comprehensive guide to viral hepatitis: causes, symptoms, transmission, diagnosis, treatment, and prevention strategies for A, B, C, D, and E.
Author: Dermatological Society of New Zealand
Revised: January 2026
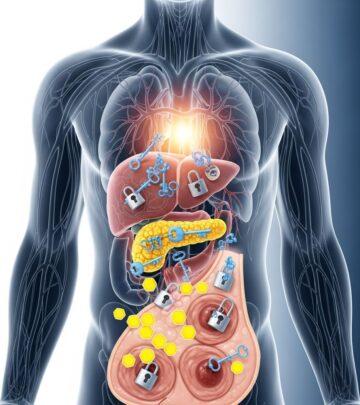
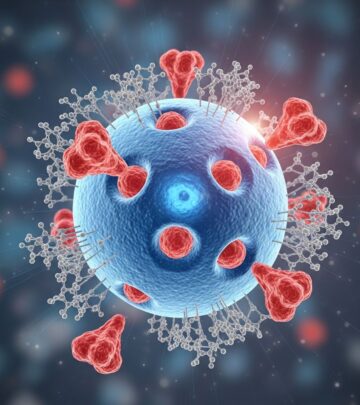
Viral hepatitis refers to liver inflammation caused by hepatotropic viruses, primarily hepatitis A, B, C, D, and E viruses (HAV, HBV, HCV, HDV, HEV). These infections can be acute or chronic, leading to symptoms like jaundice, fatigue, and potentially severe complications such as cirrhosis or liver cancer. Transmission occurs via fecal-oral route for HAV and HEV, and blood or bodily fluids for HBV, HCV, and HDV.
What is viral hepatitis?
Viral hepatitis encompasses infections by five main viruses that target the liver: HAV, HBV, HCV, HDV, and HEV. These pathogens cause hepatocyte damage, resulting in inflammation that impairs liver function. Acute infections often resolve spontaneously, but HBV, HCV, and HDV can persist chronically, increasing risks of fibrosis, cirrhosis, hepatocellular carcinoma, and liver failure. Globally, viral hepatitis affects millions, with HBV and HCV responsible for most chronic cases. Symptoms range from asymptomatic to severe, including jaundice (yellowing of skin and eyes), dark urine, and abdominal pain.
Who gets viral hepatitis?What causes viral hepatitis?
The primary causes are RNA viruses (HAV, HEV, HDV) and DNA virus (HBV), with HCV being an RNA flavivirus. HAV and HEV spread fecally-orally via contaminated food, water, or close contact. HBV, HCV, and HDV transmit parenterally through blood, semen, or perinatal routes. Non-viral causes exist but are excluded here; focus remains on viral etiologies.
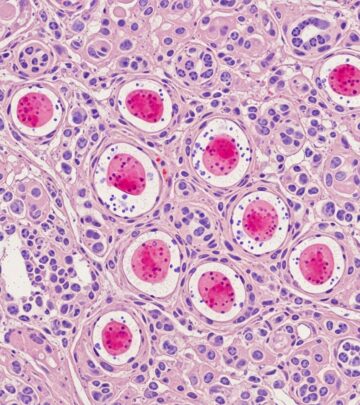
What are the clinical features of viral hepatitis?
Incubation periods differ: HAV (15–50 days), HBV (30–180 days), HCV (2–26 weeks), HEV (15–60 days). Acute phase symptoms include:
- Fatigue and weakness
- Nausea, vomiting, anorexia
- Low-grade fever, myalgias
- Dark urine, pale stools
- Jaundice, pruritus
- Right upper quadrant pain
Chronic infections (HBV, HCV, HDV) may be asymptomatic initially but progress to fatigue, arthralgias, or extrahepatic manifestations like cryoglobulinemia (HCV) or polyarteritis nodosa (HBV). Fulminant hepatitis is rare but life-threatening, with encephalopathy and coagulopathy.
How is the diagnosis of viral hepatitis made?
Diagnosis combines serology, PCR, and liver tests. Key markers:
| Virus | Acute Markers | Chronic Markers |
|---|---|---|
| HAV | IgM anti-HAV | None (self-limited) |
| HBV | HBsAg, IgM anti-HBc | HBsAg >6 months, HBeAg, HBV DNA |
| HCV | Anti-HCV, HCV RNA | HCV RNA >6 months |
| HDV | Anti-HDV, HDV RNA (with HBV) | Persistent anti-HDV |
| HEV | IgM anti-HEV, HEV RNA | Rare chronicity |
Liver biopsy assesses fibrosis in chronic cases; imaging (ultrasound, FibroScan) monitors complications.
What is the treatment for viral hepatitis?
Hepatitis A
Supportive care: rest, hydration, nutrition. Avoid hepatotoxins. Recovery typical in weeks; no antivirals needed.
Hepatitis B
Acute: Supportive (rest, fluids, analgesics). Most resolve.
Chronic: Nucleos(t)ide analogues (tenofovir, entecavir) or pegylated interferon suppress replication, prevent progression. Monitor ALT, HBV DNA.
Hepatitis C
Direct-acting antivirals (DAAs) like sofosbuvir/velpatasvir cure >95% in 8–12 weeks. Genotype testing guides therapy.
Hepatitis D
Pegylated interferon ± HBV antivirals; bulevirtide approved in some regions. Liver transplant for end-stage.
Hepatitis E
Supportive; ribavirin for chronic cases in immunocompromised.
What is the outcome for viral hepatitis?
HAV/HEV: Excellent, full recovery.
HBV acute: 90–95% resolve; 5–10% chronic (higher in neonates).
HCV: 15–25% acute resolve; 75–85% chronic.
HDV: Often chronic, aggressive course.
Complications: Cirrhosis (20–30% chronic HBV/HCV), HCC, death. Early treatment improves prognosis.
How can viral hepatitis be prevented?
- HAV/HEV: Vaccines (HAV), sanitation, safe water/food.
- HBV: Universal vaccination (3 doses), safe sex, sterile needles.
- HCV/HDV: Blood screening, harm reduction, no vaccine.
Post-exposure prophylaxis: HBIG + vaccine for HBV; immune globulin for HAV.
Related topics
- Drug-induced liver injury
- Alcoholic hepatitis
- Autoimmune hepatitis
- Cirrhosis
- Hepatocellular carcinoma
Frequently asked questions
Q: Is viral hepatitis contagious?
A: Yes, via specific routes: fecal-oral (A,E), blood/body fluids (B,C,D).
Q: Can hepatitis B be cured?
A: Acute yes; chronic managed but not cured.
Q: Is there a vaccine for hepatitis C?
A: No, prevention focuses on risk avoidance.
Q: What does jaundice indicate in hepatitis?
A: Bilirubin buildup from liver dysfunction.
Q: How long does acute hepatitis last?
A: Typically <6 months; supportive care suffices.
References
- Viral Hepatitis… Types… Symptoms… Treatment — Ministry of Health, Saudi Arabia. 2023. https://www.moh.gov.sa/en/awarenessplateform/VariousTopics/Documents/Viral%20Hepatitis%E2%80%A6%20Types%E2%80%A6%20Symptoms%E2%80%A6%20Treatment.pdf
- The Different Types of Hepatitis — UCLA Medical School. 2024. https://medschool.ucla.edu/news-article/the-different-types-of-hepatitis
- Viral Hepatitis: What It Is, Symptoms, Causes & Treatment — Cleveland Clinic. 2025-01-15. https://my.clevelandclinic.org/health/diseases/4245-hepatitis-viral-hepatitis-a-b–c
- Guide to Viral Hepatitis — Columbia Surgery. 2024. https://columbiasurgery.org/conditions-and-treatments/hepatitis
- Hepatitis: Types & Symptoms — American Liver Foundation. 2025. https://liverfoundation.org/about-your-liver/facts-about-liver-disease/hepatitis/
- Types of Viral Hepatitis — National Institute on Drug Abuse (NIDA). 2024-06-12. https://nida.nih.gov/research-topics/viral-hepatitis-very-real-consequence-substance-use/types-viral-hepatitis
- Viral Hepatitis Basics — Centers for Disease Control and Prevention (CDC). 2025-09-01. https://www.cdc.gov/hepatitis/about/index.html
Read full bio of medha deb