Vitiligo
Comprehensive guide to vitiligo: causes, symptoms, diagnosis, treatments, and management strategies for this autoimmune skin condition.

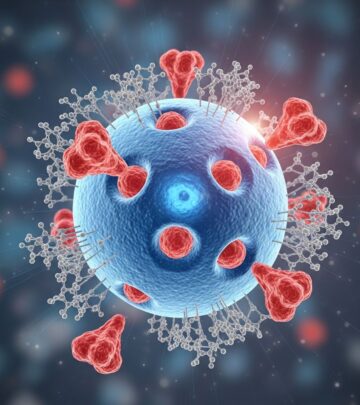
Vitiligo is a chronic autoimmune skin disorder characterised by patches of skin losing their pigment. The affected skin looks white because it contains no melanin produced by melanocytes, the pigment-making cells. It affects approximately 1% of the world’s population and can significantly impact quality of life due to cosmetic concerns and psychological effects.
What is vitiligo?
Vitiligo occurs when melanocytes in the skin are destroyed, leading to depigmented patches. This destruction is primarily autoimmune, where the body’s immune system attacks these cells. The condition can affect any part of the body, including hair, the inside of the mouth, and eyes. Patches often start small but can spread and merge over time. Vitiligo is not contagious or life-threatening but can cause emotional distress due to visible changes in appearance.
Who gets vitiligo?
Vitiligo affects people of all ages, races, and genders equally, though it is more noticeable in those with darker skin tones. Onset is common between ages 10–30, but it can occur at any time. Family history increases risk, with up to 20–30% of cases having a relative with vitiligo or other autoimmune diseases like thyroid disorders. It is associated with other autoimmune conditions, including type 1 diabetes, rheumatoid arthritis, and pernicious anaemia.
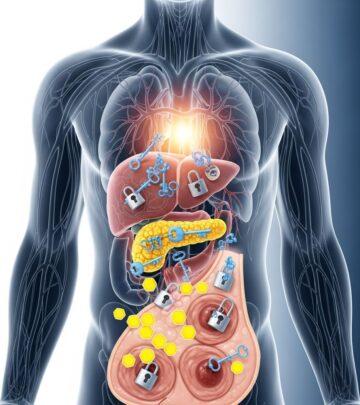
What causes vitiligo?
The exact cause is multifactorial, involving genetic predisposition, autoimmune mechanisms, oxidative stress, and environmental triggers. Key theories include:
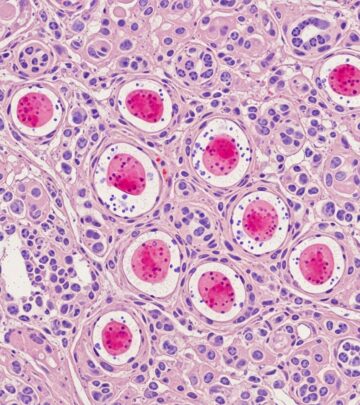
- Autoimmune destruction: T-cells attack melanocytes, confirmed by perifollicular lymphocytic infiltrates at lesion edges.
- Genetic factors: Over 30 genes linked, including those for immune regulation.
- Triggers: Sunburn, skin trauma (Koebner phenomenon), chemicals, or stress can initiate or exacerbate patches.
- Oxidative stress: Accumulation of free radicals damages melanocytes.
Associated conditions include thyroid disease (up to 30% of patients), alopecia areata, and uveitis.
What are the clinical features of vitiligo?
Vitiligo presents as well-demarcated white patches, often symmetrical. Common sites include face, neck, hands, body folds, and genitalia. Hair in affected areas may turn white (poliosis). Patches are milk-white under Wood’s lamp. Progression varies: stable for years or rapidly spreading. Itch is rare unless active spreading.
How is vitiligo diagnosed?
Diagnosis is clinical, based on history and examination. Dermatologists use:
- Wood’s lamp (UV light): Makes depigmented areas fluoresce bright white, aiding detection of subtle patches.
- Medical history: Family history, autoimmune diseases, triggers.
- Blood tests: For thyroid function, autoantibodies, ruling out other conditions.
- Skin biopsy: Rarely needed; shows absent melanocytes.
- Eye exam: For uveitis.
Differential diagnoses include pityriasis alba, tinea versicolor, post-inflammatory hypopigmentation, and melanoma regression.
What is the treatment for vitiligo?
No cure exists, but treatments aim to halt progression, promote repigmentation, or even skin tone. Choice depends on extent, stability, and patient preference. Early intervention yields better results.
Topical treatments
- Corticosteroids: First-line; potent topicals like clobetasol for face/body. Effective in 50–75% for repigmentation, used 2–3 months with monitoring for side effects like atrophy.
- Calcineurin inhibitors: Tacrolimus (0.1%) or pimecrolimus ointment; safe for face, children. Blocks T-cell activation.
- Vitamin D analogues: Calcipotriene combined with steroids enhances repigmentation.
- JAK inhibitors: Topical ruxolitinib (Opzelura™), FDA-approved; inhibits inflammatory pathways, effective in trials.
Phototherapy
Light therapy stimulates melanocyte migration. Types include:
- Narrowband UVB (NB-UVB): 2–3 sessions/week; 70% response rate, 6–12 months for results.
- PUVA (Psoralen + UVA): Oral/topical psoralen + UVA; effective for widespread disease but higher side effects.
- Excimer laser (308nm): Targeted for small areas; faster results.
Combination with topicals improves outcomes.
Systemic treatments
- Oral corticosteroids: Mini-pulse therapy for rapidly progressing vitiligo.
- Immunosuppressants: Methotrexate or ciclosporin for unstable cases.
Surgical options
For stable, segmental vitiligo (>1 year no change):
- Grafts: Punch, suction blister, split-thickness skin grafts.
- Cellular suspensions: Non-cultured melanocyte-keratinocyte transplants (e.g., ReCell®).
- Success rates 70–90% in selected patients.
Depigmentation
For extensive (>50% body) vitiligo: Monobenzone cream bleaches remaining pigment to match white areas. Permanent, requires lifelong sun protection.
Camouflage and adjuncts
- Cosmetic cover-ups, self-tanners, micropigmentation (tattooing).
- Sunscreen (SPF 50+) to prevent burns on depigmented skin.
- Counselling for psychological impact.
Types of vitiligo
| Type | Features | Prevalence |
|---|---|---|
| Non-segmental (generalised) | Symmetrical patches on both sides; most common. | 85–90% |
| Segmental | Unilateral, dermatomal distribution; stable after 1–2 years. | 10% |
| Focal | One or few patches. | Rare |
| Universal | Rare | |
| Mucosal | Lips, genitals only. | Rare |
Complications
Beyond cosmetic: sunburn risk, premature greying, eye inflammation (uveitis), hearing issues (rare). Increased thyroid disease risk requires screening. Psychological effects include depression, anxiety; support groups recommended.
Prevention and prognosis
No prevention, but trauma avoidance and prompt treatment help. Prognosis varies: facial lesions repigment best (75%), hands/Feet poorest (20%). Relapse common; maintenance therapy needed.
Frequently asked questions
Q: Is vitiligo hereditary?
A: Genetic factors contribute, but it’s not directly inherited; 20–30% familial risk.
Q: Can vitiligo be cured?
A: No cure, but treatments restore colour in many; repigmentation may fade.
Q: Does sun exposure help or harm vitiligo?
A: Depigmented skin burns easily; strict sun protection essential. Controlled phototherapy helps.
Q: Is vitiligo linked to other diseases?
A: Yes, especially autoimmune thyroiditis; annual screening advised.
Q: Can children get vitiligo?
A: Yes, often rapid onset; topical treatments safe.
References
- Vitiligo: Diagnosis, Treatment, and Steps to Take — NIAMS, NIH. 2023. https://www.niams.nih.gov/health-topics/vitiligo/diagnosis-treatment-and-steps-to-take
- Vitiligo: Diagnosis and treatment — American Academy of Dermatology (AAD). 2024. https://www.aad.org/public/diseases/a-z/vitiligo-treatment
- Vitiligo – StatPearls — NCBI Bookshelf, NIH. 2023-11-20. https://www.ncbi.nlm.nih.gov/books/NBK559149/
- Vitiligo | Department of Dermatology — UC Davis Health. 2024. https://health.ucdavis.edu/dermatology/specialties/medical/vitiligo.html
- Vitiligo: Types, Symptoms, Causes, Treatment & Recovery — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/diseases/12419-vitiligo
- Vitiligo – Treatment — NHS. 2023. https://www.nhs.uk/conditions/vitiligo/treatment/
- Vitiligo – Diagnosis & treatment — Mayo Clinic. 2024. https://www.mayoclinic.org/diseases-conditions/vitiligo/diagnosis-treatment/drc-20355916
Read full bio of medha deb