Vulvitis: Causes, Symptoms, and Treatment Options
Understanding vulvitis: comprehensive guide to causes, symptoms, and effective treatment strategies.
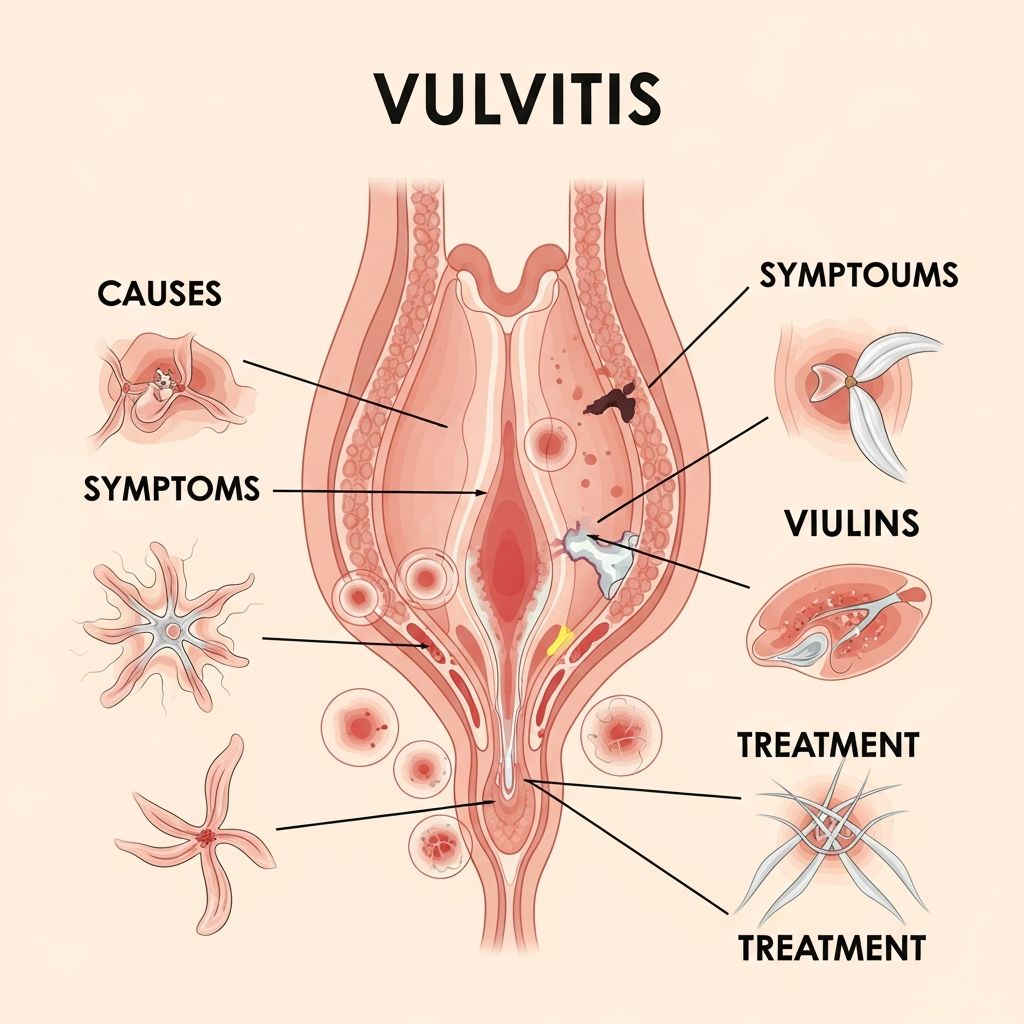
Vulvitis is an inflammation of the vulva, the external female genitalia. While it may seem alarming, vulvitis is a common condition that affects many women at various stages of life. Rather than being a disease itself, vulvitis is typically a symptom of an underlying condition or irritant. Understanding what causes vulvitis, recognizing its symptoms, and knowing the available treatment options can help you manage this uncomfortable condition effectively and seek appropriate medical care when needed.
What Is Vulvitis?
Vulvitis refers to the inflammation and irritation of the vulva, which includes the labia majora, labia minora, clitoris, and the opening of the vagina. The vulva is a particularly sensitive area of the body, which makes it susceptible to various irritants and infections. When inflammation occurs in this region, it can cause significant discomfort and concern. However, it’s important to note that vulvitis itself is not a distinct disease but rather a symptom indicating that something is irritating or infecting the vulvar tissue.
The condition is remarkably common and affects women across all age groups, from prepubescent girls to postmenopausal women. Each age group may experience vulvitis for different reasons, and the underlying causes can vary significantly. What remains consistent is that once the irritant or infection is identified and treated appropriately, most cases of vulvitis resolve relatively quickly with proper care.
Understanding the Symptoms of Vulvitis
Recognizing the symptoms of vulvitis is the first step toward seeking appropriate treatment. The symptoms can vary in intensity and presentation from person to person, but several common signs indicate vulvar inflammation:
Primary symptoms include:
– Intense itching in the vulvar area, which may be constant or intermittent- Redness and visible swelling of the labia and surrounding vulvar tissue- A burning sensation, particularly during urination or sexual intercourse- Abnormal vaginal discharge that may vary in color, consistency, or odor- Soreness and general discomfort in the genital region- Visible blisters, lesions, or skin changes on the vulva
These symptoms can range from mild to severe and may develop gradually or appear suddenly. Some women experience only one or two symptoms, while others may have multiple symptoms occurring simultaneously. It’s important not to ignore these symptoms or attempt self-diagnosis, as various conditions can cause similar presentations, and appropriate medical evaluation is necessary for proper treatment.
Common Causes of Vulvitis
Vulvitis can develop from numerous causes, which healthcare providers typically categorize into infections, irritants, allergies, hormonal factors, and dermatological conditions. Understanding these causes is essential for both prevention and appropriate treatment.
Infectious Causes
Infections represent one of the most common causes of vulvitis. Various microorganisms can invade vulvar tissue and cause inflammation. Bacterial vaginosis, a common vaginal infection caused by an imbalance of normal bacteria, frequently extends to the vulva causing irritation and discharge. Yeast infections, particularly those caused by Candida albicans, produce intense itching and visible inflammation along with characteristic thick, white discharge.
Viral infections such as herpes simplex virus can cause painful blisters and significant vulvar inflammation. Sexually transmitted infections, including gonorrhea and chlamydia, may cause vulvitis as part of a broader genital infection. Additionally, parasitic infections such as scabies and pubic lice can cause severe itching and vulvar irritation. Viral warts (human papillomavirus) may also affect the vulva and cause localized inflammation and discomfort.
Irritant and Allergic Causes
Many everyday products and habits can irritate the sensitive vulvar skin. Common culprits include perfumed soaps, douches, and vaginal sprays that disrupt the natural vulvar environment. Fabric softeners and laundry detergents, particularly heavily scented varieties, can cause dermatitis when they come into contact with vulvar skin. Synthetic underwear that doesn’t allow proper air circulation can trap moisture and create an environment conducive to irritation.
Chlorine in swimming pools and hot tubs frequently causes vulvar irritation, particularly in women with sensitive skin. Spermicidal products, both in contraceptive foams and on lubricated condoms, can trigger allergic reactions. Sanitary napkins and panty liners, especially those with deodorants or fragrances, may cause irritation in susceptible individuals. Even prolonged contact with moisture, such as wearing a wet bathing suit for extended periods, can lead to maceration and vulvitis.
Hormonal Causes
Estrogen plays a crucial role in maintaining vulvar and vaginal tissue health. During menopause, estrogen levels decline significantly, leading to vaginal atrophy and vulvar irritation. This condition, known as atrophic vaginitis or genitourinary syndrome of menopause, causes the vulvar and vaginal tissues to become thin, dry, and easily irritated. Young girls who have not yet reached puberty may also experience vulvitis due to low estrogen levels, often accompanied by soreness, redness, and sometimes vaginal discharge.
Dermatological Conditions
Chronic skin conditions frequently affect the vulva as well as other body areas. Eczema and dermatitis can cause persistent vulvar inflammation and itching. Psoriasis may present on the vulva with characteristic plaques and irritation. Lichen sclerosus is a chronic inflammatory condition that causes white patches, itching, and potential tissue changes. These conditions may require specialized dermatological treatment in addition to general vulvar care measures.
Diagnosis of Vulvitis
Proper diagnosis of vulvitis involves a comprehensive evaluation by a healthcare provider. Your doctor will begin by reviewing your medical history and asking detailed questions about your symptoms, including when they started, their severity, and any potential triggers you’ve noticed. Questions about personal hygiene practices, recent product changes, sexual activity, and menstrual history provide important diagnostic clues.
A physical examination follows, during which your healthcare provider will visually inspect the vulva and surrounding area for signs of inflammation, such as redness, swelling, blisters, or lesions. A complete pelvic examination may be performed to assess the vagina and cervix. Your provider may take a sample of vaginal fluid to examine under a microscope, looking for signs of infection such as yeast cells, bacterial overgrowth, or other microorganisms.
Depending on the suspected cause, additional tests may be ordered. These might include vaginal cultures to identify specific bacterial or fungal organisms, tests for sexually transmitted infections, or other specialized testing. Once your healthcare provider determines the underlying cause of your vulvitis, they can recommend targeted treatments to address the specific problem.
Treatment Strategies for Vulvitis
Treatment for vulvitis depends entirely on its underlying cause. However, several general principles apply across most cases, and many treatment approaches can be used together for optimal relief.
Self-Care and Preventive Measures
One of the most important steps in treating vulvitis is removing or avoiding the irritating factor. If a specific product or habit is causing irritation, discontinuing its use is essential. Additionally, implementing proper vulvar care practices can significantly improve symptoms:
– Wash the vulva once daily using only warm water, avoiding soaps and cleansing products- Wear cotton underwear that is loose-fitting and breathable- Avoid tight clothing such as pantyhose or restrictive pants- Change out of wet clothing, including swimsuits and workout attire, promptly- Use unscented, dye-free toilet paper- Avoid douching and vaginal sprays entirely- Apply emollient creams to help soothe and protect the skin- Avoid spermicidally lubricated condoms- Take sitz baths with warm water, optionally with soothing compounds like colloidal oatmeal
Topical Steroid Creams
Topical corticosteroid creams are frequently prescribed for vulvitis, particularly when inflammation is significant. These medications work by reducing inflammation and irritation, providing considerable relief for many women. Steroid creams come in various strengths, and healthcare providers typically begin with the weakest strength appropriate for the condition. If this proves ineffective, stronger formulations may be prescribed. These creams should be used as directed and typically for short durations to avoid potential side effects from prolonged steroid use on sensitive genital tissue.
Hormonal Treatments
For women experiencing vulvitis due to low estrogen levels, particularly postmenopausal women or those with atrophic vaginitis, estrogen creams, pessaries, or vaginal tablets may be prescribed. These treatments deliver estrogen directly to the vulvar and vaginal tissues, helping to restore tissue thickness, elasticity, and natural moisture. Systemic hormone replacement therapy may also be considered depending on individual circumstances and preferences.
Anti-Infection Medications
When vulvitis results from an infectious cause, specific anti-infective medications are prescribed. For fungal infections like yeast, antifungal creams or oral medications such as fluconazole may be recommended. Bacterial infections are typically treated with appropriate antibiotics, either topical or oral depending on severity. Viral infections may require antiviral therapy, while parasitic infections need specific antiparasitic treatments. It’s crucial to use the correct medication for the identified cause, as using the wrong treatment can worsen symptoms and prolong the condition.
Specialized Treatments
For certain chronic vulvar conditions, specialized treatments may be necessary. Vulvodynia, characterized by chronic vulvar pain without an obvious cause, may require local anesthetic creams for symptom relief along with other pain management strategies. Some dermatological conditions affecting the vulva may require specific treatments targeting the underlying skin disorder. In rare cases where vulvar lesions or abnormal tissue changes are present, surgical excision may be necessary, though this is typically reserved for specific indications.
When to Seek Medical Care
While many cases of mild vulvitis resolve with self-care measures and home remedies, it’s important to recognize when professional medical evaluation is necessary. Schedule a visit with your healthcare provider if you experience vulvar symptoms that persist beyond a few days, if symptoms are severe or interfering with daily activities, or if you’re unsure about the cause of your symptoms. Additionally, seek care if over-the-counter treatments haven’t helped, if you’ve never experienced these symptoms before, or if symptoms recur frequently.
It’s particularly important not to self-treat with over-the-counter antifungal or anti-itch products without professional guidance. Using the wrong treatment can actually worsen vulvitis and delay proper healing. Your healthcare provider can accurately identify the cause and recommend appropriate treatment, which typically leads to resolution within weeks of starting the correct therapy.
Prevention of Vulvitis
Many cases of vulvitis can be prevented by adopting healthy vulvar care habits and avoiding known irritants. The same practices used to treat vulvitis effectively prevent its recurrence. Maintaining good genital hygiene using only water, wearing breathable cotton underwear, avoiding irritating products, and being mindful of potential allergens can significantly reduce your risk of developing vulvitis. Women experiencing recurrent vulvitis should work with their healthcare provider to identify specific triggers and develop a personalized prevention strategy.
Frequently Asked Questions About Vulvitis
Q: Is vulvitis contagious?
A: Vulvitis itself is not contagious, but some of its causes are. Infections like bacterial vaginosis, yeast infections, and sexually transmitted infections that cause vulvitis can be transmitted to partners. However, vulvitis resulting from allergies, irritants, or skin conditions is not contagious.
Q: Can vulvitis go away on its own?
A: Mild vulvitis caused by irritation may resolve with self-care and removal of the irritant. However, vulvitis caused by infections typically requires medical treatment. Without appropriate treatment, vulvar inflammation can progress to more serious infections. It’s best to consult a healthcare provider for accurate diagnosis and treatment.
Q: How long does vulvitis typically take to resolve?
A: With appropriate treatment, most cases of vulvitis resolve within weeks. The timeline depends on the underlying cause and how quickly treatment is initiated. Some cases may improve within days with proper self-care, while others requiring medication may take two to four weeks for complete resolution.
Q: Can I use over-the-counter yeast infection treatments for vulvitis?
A: No. Over-the-counter antifungal creams are only appropriate if you’ve been diagnosed with a yeast infection. Using these products for other causes of vulvitis can worsen symptoms. Always have your symptoms properly evaluated by a healthcare provider before starting any treatment.
Q: What should I avoid during treatment for vulvitis?
A: Avoid all irritating products including scented soaps, douches, perfumed toilet paper, and fabric softeners. Also avoid sexual intercourse until symptoms resolve, wear only cotton underwear, avoid tight clothing, and don’t use over-the-counter anti-itch products unless specifically recommended by your healthcare provider.
Q: Is vulvitis common in young girls?
A: Yes, vulvitis can occur in prepubescent girls, often due to low estrogen levels before puberty. It may present as redness, soreness, and sometimes vaginal discharge. Maintaining good hygiene practices and avoiding irritants can help prevent vulvitis in young girls, and medical evaluation is important if symptoms persist.
References
- Vulvitis: Causes, Symptoms, and Treatments — Cleveland Clinic. 2024. https://my.clevelandclinic.org/health/diseases/15175-vulvitis
- Vulvitis — University of Rochester Medical Center. 2024. https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=85&contentid=p00596
- Vulvitis: Causes, Symptoms, Treatment — Baptist Health. 2024. https://www.baptisthealth.com/care-services/conditions-treatments/vulvitis
- Vulvitis | Causes, Symptoms, and Treatments — Patient.info. 2024. https://patient.info/womens-health/vulval-problems-leaflet/vulvitis
- Vaginitis — Symptoms and Causes — Mayo Clinic. 2024. https://www.mayoclinic.org/diseases-conditions/vaginitis/symptoms-causes/syc-20354707
Read full bio of Sneha Tete











