Postnatal OCD: Symptoms, Treatment, And Support For New Parents
Personal stories and expert insights reveal the hidden struggles of postnatal OCD, a treatable condition affecting new parents.

What It’s Like to Have Postnatal OCD
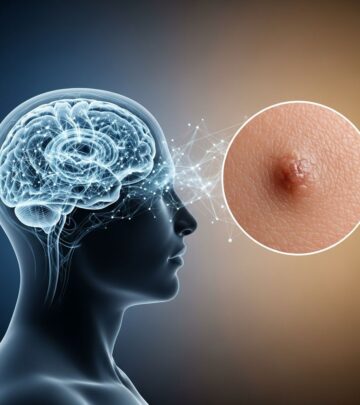
Postnatal obsessive-compulsive disorder (OCD) is a perinatal mental health condition that can emerge after childbirth, characterized by intrusive, distressing thoughts and compulsive behaviors centered around the baby’s safety. Unlike common myths, individuals with postnatal OCD do not act on these thoughts and are not dangerous to their infants; the thoughts are ego-dystonic, meaning they conflict with the person’s values and cause profound anxiety.
Understanding Postnatal OCD: More Than Just Worry
Postnatal OCD, also known as postpartum OCD, affects new parents, primarily mothers, but can impact fathers and non-birthing parents too. It involves
obsessions
—unwanted, persistent thoughts, images, or urges that provoke intense fear—andcompulsions
—repetitive behaviors or mental acts performed to neutralize the anxiety. Common obsessions include fears of harming the baby accidentally or intentionally, contaminating the baby with germs, or losing control and dropping the baby. Compulsions might involve excessive checking, cleaning, or avoidance of the baby to prevent perceived harm.Research indicates that women are at increased risk for OCD onset or exacerbation during the perinatal period. A study notes rapid symptom onset, often within 2-4 weeks postpartum, distinguishing it from general OCD. Up to 70-100% of new parents experience some intrusive thoughts, but in postnatal OCD, these escalate into a disorder disrupting daily life and parent-infant bonding.
Symptoms: The Intrusive Thoughts That Haunt New Parents
The hallmark of postnatal OCD is
intrusive thoughts
about the baby’s harm, such as stabbing, drowning, or shaking the infant—these are taboo fears that horrify the parent. Unlike psychosis, individuals retain insight that these thoughts are irrational and resist acting on them.- Fear of harm: Thoughts of accidentally harming the baby while bathing, feeding, or holding them.
- Contamination obsessions: Intense worry about germs infecting the baby, leading to hours of cleaning.
- Checking compulsions: Repeatedly verifying the baby’s breathing, safety straps, or that doors are locked.
- Avoidance: Staying away from the baby to prevent ‘dangerous’ scenarios, impairing bonding.
- Mental rituals: Praying, repeating phrases, or mentally reviewing actions to avert catastrophe.
These symptoms cause severe anxiety, exhaustion, and isolation. Sleep deprivation exacerbates them, creating a vicious cycle.
Causes and Risk Factors: Why Does It Happen?
The exact etiology is multifactorial, blending biological, psychological, and environmental elements.
Biological Factors
- Hormonal shifts: Dramatic drops in estrogen and progesterone post-delivery disrupt brain chemistry, particularly serotonin pathways linked to OCD.
- Neurotransmitter imbalances: Dysregulation of serotonin and dopamine contributes to obsessions and compulsions.
- Genetic predisposition: Family history of OCD, anxiety, or depression heightens vulnerability.
Psychological and Environmental Triggers
- Sleep deprivation and stress: Newborn care demands amplify anxiety.
- Traumatic birth: Complications or difficult deliveries can trigger onset.
- Prior mental health: Pre-existing anxiety or OCD increases risk.
- Societal pressures: ‘Perfect mother’ ideals fuel self-doubt.
These factors converge in the vulnerable postpartum window, making early identification crucial.
Differential Diagnosis: OCD vs. Depression, Anxiety, or Psychosis
Postnatal OCD often overlaps with postpartum depression (PPD) or anxiety but is distinguished by ego-syntonic obsessions and compulsions. Key differentiators:
| Condition | Key Features | Insight Level |
|---|---|---|
| Postnatal OCD | Intrusive harm thoughts, compulsions (checking/cleaning), anxiety relief from rituals | Full insight: knows thoughts are irrational |
| Postpartum Depression | Persistent sadness, low mood, fatigue, possible intrusive thoughts without compulsions | Insight present, but mood dominates |
| Postpartum Anxiety | General worry, panic attacks, without specific obsessions/compulsions | Insight present |
| Postpartum Psychosis | Delusions, hallucinations, loss of insight, potential to act on thoughts | Poor/no insight: believes thoughts are real |
Rapid onset post-birth and preserved reality-testing guide diagnosis. Psychoeducation reassures parents they are unlikely to harm their baby.
Treatment Options: Proven Paths to Recovery
Postnatal OCD is highly treatable, with
first-line treatments
mirroring general OCD protocols, adapted for perinatal safety.Cognitive Behavioral Therapy (CBT) with Exposure and Response Prevention (ERP)
**ERP** is the gold standard: patients face obsessions without compulsions, reducing anxiety over time. For example, a mother fearing contamination might touch a ‘dirty’ object without washing, building tolerance. Sessions are tailored to avoid baby distress.
Medication
**SSRIs** like sertraline, fluoxetine, or citalopram (at higher OCD doses) are safe for breastfeeding, per guidelines. Combine with ERP for optimal outcomes. Clomipramine is an alternative. Consult providers for risks/benefits.
Supportive Interventions
- Psychoeducation: Understanding OCD reduces shame.
- Partner involvement: Educate family to support without enabling compulsions.
- Lifestyle: Prioritize sleep, mindfulness, stress reduction.
- Hormone therapy: For imbalances, bio-identical options under endocrinologist care.
Early intervention (within weeks) prevents chronicity and aids bonding.
Personal Stories: Living with Postnatal OCD
Imagine the terror: a new mother, exhausted, visualizes shaking her crying baby to silence it. She avoids holding her infant, checks breathing obsessively, and cleans nonstop, convinced she’s a monster. This mirrors Mrs. M’s case, who after birth developed harm obsessions, avoided her baby, and responded fully to high-dose citalopram and ERP.
Another parent describes: ‘The thoughts screamed I’d drop her down stairs. I couldn’t be alone with her.’ Recovery involved therapy confronting fears, rebuilding confidence. These stories highlight isolation but also hope—most recover fully.
Challenges in Diagnosis and Seeking Help
Stigma silences sufferers fearing judgment as ‘bad parents.’ Many hide symptoms, delaying treatment. Healthcare providers must screen routinely, as symptoms mimic normal worries. Barriers include guilt, lack of awareness, and access to perinatal specialists.
Recovery and Long-Term Outlook
With treatment, 70-80% achieve remission. Ongoing management prevents relapse, especially with stressors. Strong support networks foster resilience. Post-recovery, parents often bond deeply, viewing OCD as a surmounted challenge.
Frequently Asked Questions (FAQs)
Can postnatal OCD make me harm my baby?
No. People with OCD recognize thoughts as irrational and avoid acting on them. Those who harm lack insight, indicating psychosis—a medical emergency.
Is medication safe while breastfeeding?
Yes, SSRIs like sertraline are generally safe; consult your doctor for monitoring.
How long does recovery take?
With ERP and meds, significant improvement in 8-12 weeks; full recovery varies.
Does it only affect mothers?
No, fathers and partners can experience it too.
What if I suspect I have it?
Contact a perinatal mental health specialist immediately for assessment.
References
- Understanding Postpartum OCD: Symptoms, Causes & Support — Balanced Wellness. 2021. https://balanced-wellness.org/blog/postpartum-ocd
- Post-Partum OCD — OCD Institute of Texas. Accessed 2026. https://ocditexas.com/post-partum-ocd/
- Postpartum Blues: Treatment Options for OCD and Depression Following Childbirth — Balanced Mental Health AZ. 2025-06-13. https://www.balancedmentalhealthaz.com/2025/06/13/postpartum-blues-treatment-options-for-ocd-and-depression-following-childbirth/
- Diagnosis and Treatment of Postpartum Obsessions and Compulsions — National Institutes of Health (PMC). 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7081835/
- Unexpected OCD Postpartum: Understanding Postpartum OCD and the Mother/Baby Attachment — Anxiety and Depression Association of America (ADAA). Accessed 2026. https://adaa.org/learn-from-us/from-the-experts/blog-posts/consumer/unexpected-ocd-postpartum
- The Difference Between Postpartum Anxiety, OCD and Psychosis — Cedars-Sinai. Accessed 2026. https://www.cedars-sinai.org/stories-and-insights/healthy-living/difference-between-postpartum-anxiety-ocd-psychosis
- Postpartum OCD Fact Sheet — International OCD Foundation (IOCDF). 2014. https://iocdf.org/wp-content/uploads/2014/10/Postpartum-OCD-Fact-Sheet.pdf
Read full bio of medha deb