Herpes Simplex
Comprehensive guide to herpes simplex virus infections, symptoms, diagnosis, treatment, and prevention strategies.
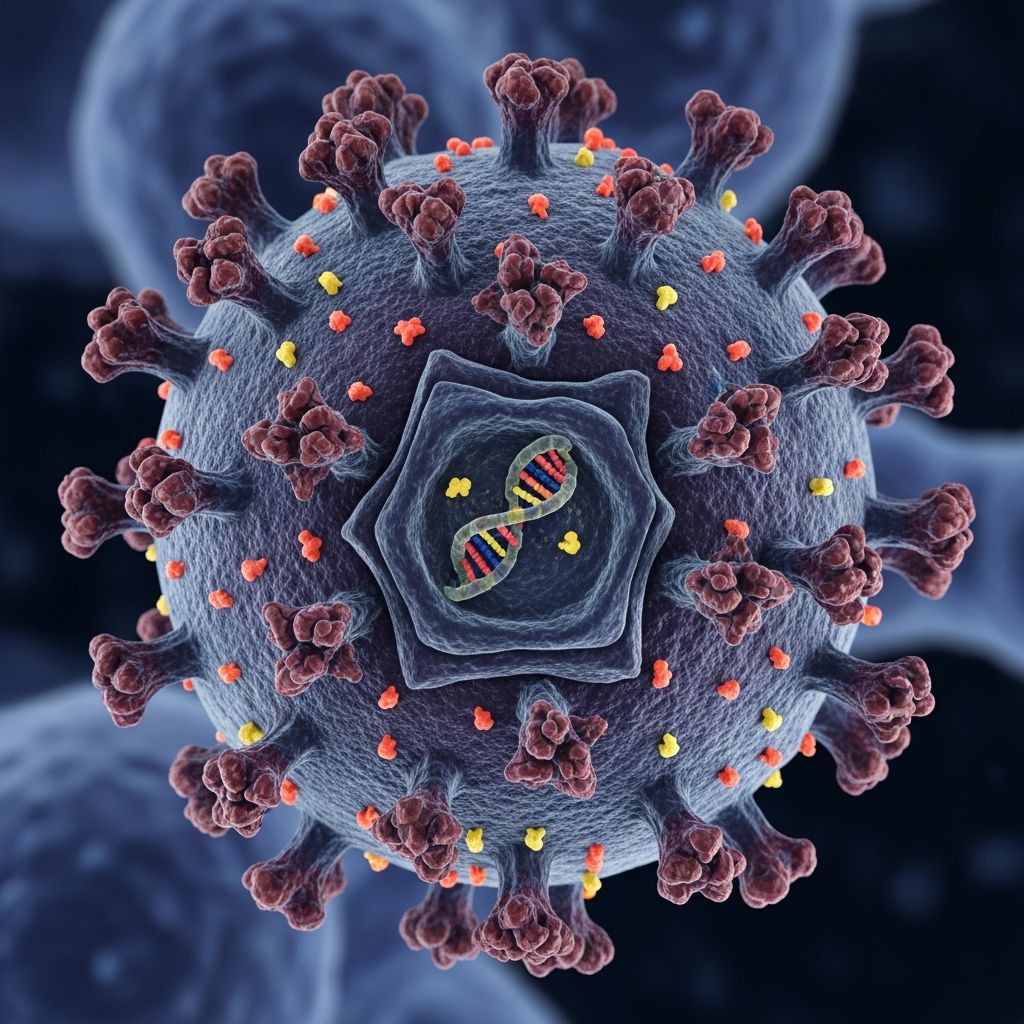
Herpes simplex is a viral infection caused by the herpes simplex virus (HSV), primarily manifesting as painful blisters or ulcers on the skin or mucous membranes, most commonly around the mouth (oral herpes) or genitals (genital herpes).
What is herpes simplex?
Herpes simplex refers to infections caused by two closely related viruses: herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2). HSV-1 typically causes oral herpes, often known as cold sores or fever blisters on or around the lips, while HSV-2 is more commonly associated with genital herpes. However, there is significant overlap; HSV-1 can cause genital infections via oral-genital contact, and HSV-2 can affect the oral region.
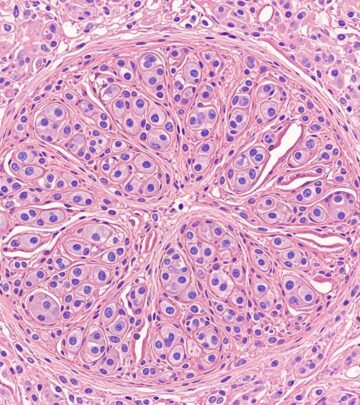
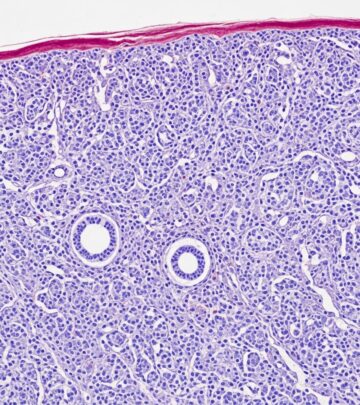
These viruses belong to the Herpesviridae family and establish lifelong latency in sensory nerve ganglia after initial infection, leading to potential recurrent outbreaks. Globally, HSV-1 seroprevalence is 50-80% in adults, and HSV-2 is 20-40%. Most infections are asymptomatic, but when symptomatic, they produce characteristic clustered vesicles on an erythematous base that evolve into ulcers.
Who gets herpes simplex?
Herpes simplex affects people of all ages, races, and sexes. HSV-1 is usually acquired in childhood through non-sexual contact like kissing, with primary infection often asymptomatic. HSV-2 is primarily sexually transmitted and more common in adults. Risk factors include multiple sexual partners, unprotected sex, and weakened immunity. Pregnant individuals with genital HSV require special management to prevent neonatal transmission.
- Children: Often get HSV-1 from family members.
- Adults: HSV-2 via sexual contact; increasing genital HSV-1 cases.
- Immunocompromised: More severe, disseminated disease.
What causes herpes simplex?
HSV-1 and HSV-2 are double-stranded DNA viruses that infect epithelial cells, replicate, and then travel retrogradely along sensory nerves to establish latency in dorsal root ganglia (trigeminal for oral, sacral for genital). Reactivation occurs due to triggers, causing anterograde transport back to the skin.
Transmission happens through direct skin-to-skin contact with infected areas, even without visible lesions (asymptomatic shedding). Common routes include:
| Type of Contact | How HSV Spreads |
|---|---|
| Genital-to-genital | HSV-2 primarily, causing genital herpes. |
| Oral-to-oral | HSV-1, causing oral herpes. |
| Oral-to-genital | HSV-1 to genitals. |
| Genital-to-oral | HSV-2 to mouth (less common). |
| Skin-to-sore | Touching active lesions. |
What are the clinical features of herpes simplex?
Primary infection
The initial (primary) episode is often the most severe, occurring 2-12 days post-exposure (incubation 1-26 days, typically 6-8). Symptoms include prodrome of tingling/itching, followed by clustered vesicles that rupture into painful ulcers, plus systemic signs like fever, lymphadenopathy, and malaise. Oral primary: gingivostomatitis with vesicles on lips, tongue, mucosa. Genital primary: vesicles on vulva, penis, perianal area; dysuria common in women.
Recurrent infection
Reactivations are milder/shorter (4-10 days), localized, with fewer lesions. Triggers: stress, UV light, illness, menstruation. Oral recurrences: labialis (cold sores). Genital: similar but less frequent over time.
Complications
- Neonatal herpes: Rare but severe; from maternal genital HSV at delivery.
- Herpetic whitlow: Finger infection from auto/contact inoculation.
- Herpes keratitis: Eye involvement, risk of vision loss.
- Encephalitis/meningitis: HSV-1 brain infection; CSF PCR diagnostic.
- Disseminated in immunocompromised.
Diagnosis of herpes simplex
Often clinical, but confirmation via lab tests.
- Viral culture: Swab fresh vesicle base; 50% sensitive, gold standard historically.
- PCR: Lesion swab or CSF; 98-100% sensitive/specific.
- Serology: Type-specific IgG (e.g., HerpeSelect); detects past infection.
- Tzanck smear: Multinucleated giant cells (less specific).
For CNS: CSF lymphocytic pleocytosis, PCR.
Treatment of herpes simplex
Antivirals shorten duration/severity; supportive care for pain/fever.
Episodic therapy (acute outbreaks)
- Acyclovir 400mg 3x/day x5-10d, or 200mg 5x/day.
- Valacyclovir 1g BID x5-10d (better bioavailability).
- Famciclovir 250mg TID x5d.
- Start within 72h of prodrome.
Suppressive therapy (frequent recurrences)
- Acyclovir 400mg BID daily.
- Valacyclovir 500mg-1g daily; reduces shedding 50%.
- Review yearly.
Special cases
- Pregnancy: Suppressive acyclovir third trimester if recurrent.
- Immunocompromised: Higher doses/IV.
- Neonatal: IV acyclovir.
Topicals (e.g., acyclovir cream) minimally effective.
What is the outcome for herpes simplex?
Lifelong infection with decreasing outbreak frequency/severity. Suppressive therapy improves quality of life, reduces transmission. No cure; vaccines in development.
How can herpes simplex be prevented?
- Condoms/dental dams reduce but don’t eliminate risk (shedding).
- Avoid contact during outbreaks/prodrome.
- Suppressive therapy for discordant couples.
- Disclose status; test partners.
- Sunscreen for oral HSV.
Herpes encephalitis
HSV-1 causes 90% cases; focal temporal lobe necrosis. Symptoms: fever, seizures, altered mental status. CSF PCR diagnostic; treat IV acyclovir 10mg/kg q8h x14-21d.
Neonatal herpes simplex
Perinatal transmission (85% vaginal delivery); SEM (skin/eye/mouth), CNS, disseminated. High mortality/morbidity. C-section if active lesions; suppressive therapy.
Frequently Asked Questions
Q: Can herpes be spread without symptoms?
A: Yes, via asymptomatic viral shedding from infected skin.
Q: Is herpes curable?
A: No, but antivirals manage symptoms and reduce transmission.
Q: Does HSV-1 cause genital herpes?
A: Yes, increasingly via oral sex; 30% genital cases.
Q: Safe to have sex with herpes?
A: Use condoms, suppressive therapy; avoid during outbreaks.
Q: Pregnancy and herpes risks?
A: Neonatal transmission risk; suppressive acyclovir recommended.
References
- Herpes Simplex Virus — BC Centre for Disease Control. Accessed 2026. https://www.bccdc.ca/health-info/diseases-conditions/herpes-simplex-virus
- Herpes Simplex Virus (HSV): Types Symptoms, & Treatment — Cleveland Clinic. Accessed 2026. https://my.clevelandclinic.org/health/diseases/22855-herpes-simplex
- Herpes Simplex Virus — Johns Hopkins ABX Guide. Accessed 2026. https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540242/all/Herpes_Simplex_Virus
- Herpes simplex infections — Primary Care Dermatology Society. 2025-07-18. https://www.pcds.org.uk/clinical-guidance/herpes-simplex
- Herpes Simplex Virus: A Practical Guide to Diagnosis, Management — PubMed. 2024. https://pubmed.ncbi.nlm.nih.gov/38331482/
- HSV: THE ULTIMATE GUIDE — HSHC. 2019. https://hshc.ca/wp-content/uploads/2019/01/FAQ-Sheet-HSV-2019.pdf
- Herpes – STI Treatment Guidelines — CDC. Accessed 2026. https://www.cdc.gov/std/treatment-guidelines/herpes.htm
Read full bio of Sneha Tete